Early Indianapolis residents lived under conditions that led to frequent bouts of malaria, typhoid fever, and cholera. Families were often large and lived in crowded cabins, with no windowpanes or screens to keep out insects. Streams were often polluted, and there were no sewage or trash collection systems. Nearby swampland was a breeding ground for disease-carrying mosquitoes.
Epidemics were common. According to one report a malaria epidemic in the summer of 1821 claimed 72, or one of eight, residents. In 1832 a cholera epidemic killed 62 people in one month. In these early years, half the children under 14 lost at least one parent to disease. Since germ theory was unknown, diseases were believed to be God’s punishment or the result of “miasmas,” invisible substances thought to rise from damp soil and night air. Draining the swamps to reduce these miasmas did reduce the number of mosquitoes, the unsuspected carriers of malaria.
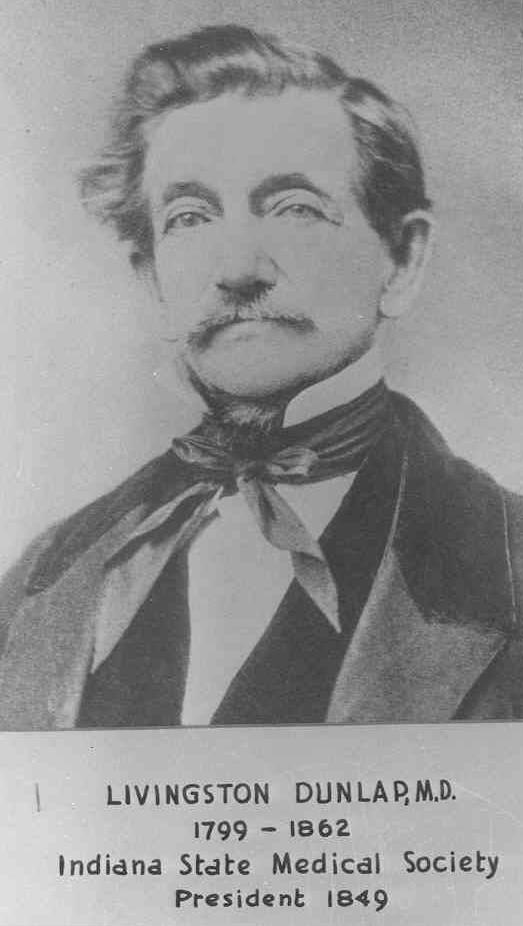
Antebellum interest in public health was very sporadic, peaking only when an epidemic struck. For example, in 1833 Dr. Livingston Dunlap first proposed a hospital for victims of cholera and smallpox. In 1847 an early board of health raised $1,000 to construct such a hospital, but interest again waned with the demise of the smallpox epidemic. Dunlap persisted in his efforts until the first city hospital was finally constructed in 1859.
The Shattuck Report (1850), a survey of sanitary conditions in Massachusetts, became a blueprint for public health efforts for decades to come. Its more than 50 recommendations on issues such as water and air pollution, control of communicable diseases, and housing construction were gradually implemented over the next century. Possibly influenced by this report, the Common Council created the first official and permanent board of health for Indianapolis in 1859. In 1863 the board adopted food inspection standards and rules for keeping and disposing of animals, and in 1871 required sewer hook-ups for hotels, restaurants, hospitals, saloons, and boardinghouses. However, in the 1880s sanitary conditions remained extremely poor. Drinking water samples were very bad, hogs and cattle were allowed to wander the city streets (until banned by city ordinance in the late 1880s), and household wastes and garbage were often thrown directly into the streets. To deal with such conditions the city adopted standards for well and water inspection in 1893 and for plumbing and garbage in 1904 and 1906.
The late 19th and early 20th centuries also witnessed the creation of public health agencies and associations. In 1879 the , an organization of women who served the poor and sick, offered the first nursing services in the city. The Public Health Nursing Association was formed in 1912 as a voluntary agency, with initial efforts focused on maternal and child health, tuberculosis, and school health issues. Early efforts in maternal and child health focused on improving milk quality. The Indianapolis Pure Milk Association members maintained the first well-baby clinics during the summers; a successor organization, the Children’s Aid Association, expanded to year-round well-baby clinics and added children’s dental clinics. The city began a school health program in 1906, added vision and hearing screening in 1911, and employed the first school nurse in 1914.
In 1896, the was seriously polluted, resulting in a typhoid epidemic. Having a clean surface water supply was critical since wells alone could not supply a city the size of Indianapolis. For this reason, the began constructing a modern filtration system in 1904 and settling basins in 1908. It first used liquid chlorine in 1916. The typhoid rate remained high for years, however, because a majority of the families in Indianapolis continued to use wells and privies. Eventually, the general improvement of sanitary standards effectively eliminated diseases such as cholera and typhoid fever.

In the early 1900s, certain contagious diseases such as tuberculosis remained widespread. Controlling tuberculosis by quarantining its victims in a “pest house” was replaced by treatment in sanitariums. In 1945 streptomycin was first used for the successful treatment of tuberculosis and by the 1950s the incidence of this disease was greatly reduced.
The Board of Health and Charities, formed in 1905, hired the city’s first full-time health officer, Dr. Elijah Elder (later secretary of the State Board of Health). Dr. Herman Morgan served in this role from 1912 until 1946 and played a major role in changing public attitudes toward public health; he helped to establish pure food regulations and supported the construction of a city sewage disposal plant. During his term, much progress was made in controlling venereal disease and in reducing pneumonia and infant death rates. From 1941 to 1946 the infant mortality rate declined from 125 to 46 per 100,000 population.
In 1948, the Health and Welfare Council, a group of 115 agencies, recommended the merger of the public health and hospital services of the city and Marion County. Three years later the General Assembly created the . Before this occurred, the 110,000 county residents outside the city limits had received very few public health services.
Modern efforts in public health have focused on infants and children. In 1954 the Division of Public Health began a polio vaccination program among school children, effectively eliminating this disease. The division began decentralizing public health services to neighborhood centers in 1960, and in 1969 implemented the nation’s first successful rubella vaccination program. In 1987 the National Children’s Defense Fund issued a report on infant mortality that cited Indianapolis as the city with the highest Black infant mortality rate in the country. The Marion County Task Force on Infant Mortality formed by the City-County Council in 1988 to study this issue led to the in 1990, which focused on comprehensive prenatal care, financial accessibility, good transportation, care coordination, and education and outreach. By the early 1990s Black infant mortality had not declined significantly, but the groundwork had been laid to remove barriers to prenatal care.
Acquired Immune Deficiency Syndrome (AIDS) became a very critical public health issue in the 1980s. In Marion County, the first case was reported in 1982, with 737 cases reported through 1992. Major environmental health issues in the 1980s were the control of hazardous materials and groundwater quality.
*Note: This entry is from the original print edition of the Encyclopedia of Indianapolis (1994). We are currently seeking an individual with knowledge of this topic to update this entry.
Help improve this entry
Contribute information, offer corrections, suggest images.
You can also recommend new entries related to this topic.
