During much of the 19th, century hospitals offered few advantages to the sick and suffering. Doctors treated most patients in their own homes. Early hospitals had evolved from almshouses and were little more than welfare institutions. The medical care at these institutions was minimal, and the death rate from infection was high (approximately 10 percent). Patients in these early hospitals were poor and had been abandoned by family and friends.
By the mid-19th century, most municipal hospitals abandoned their welfare functions and began operating as true hospitals, offering primarily medical care to the poor. A number of private, or voluntary, hospitals also provided care to the poor. Not until the late 19th and early 20th centuries did the middle class use hospital facilities.
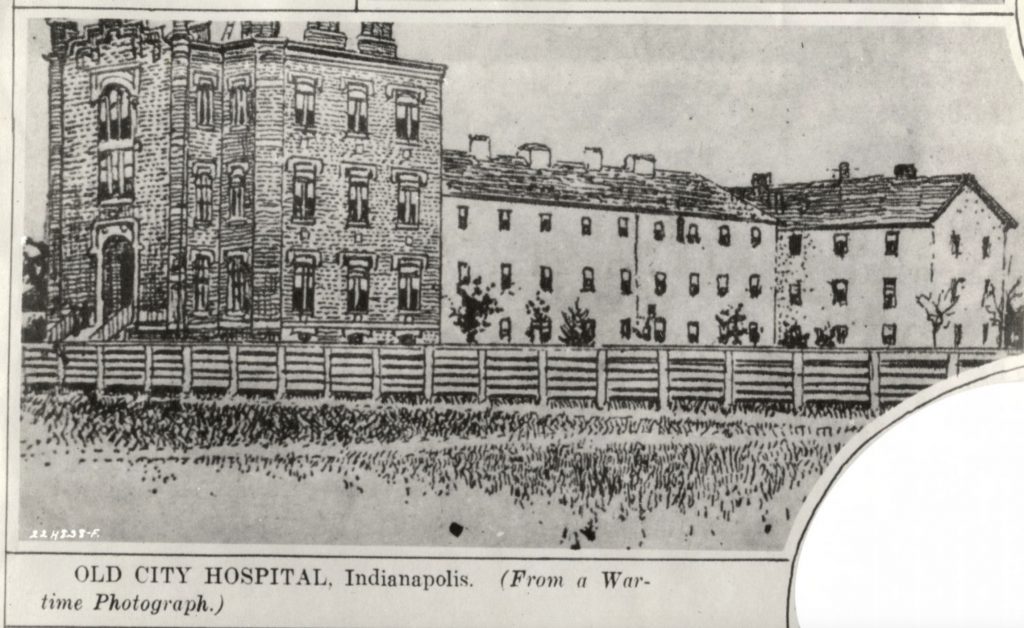
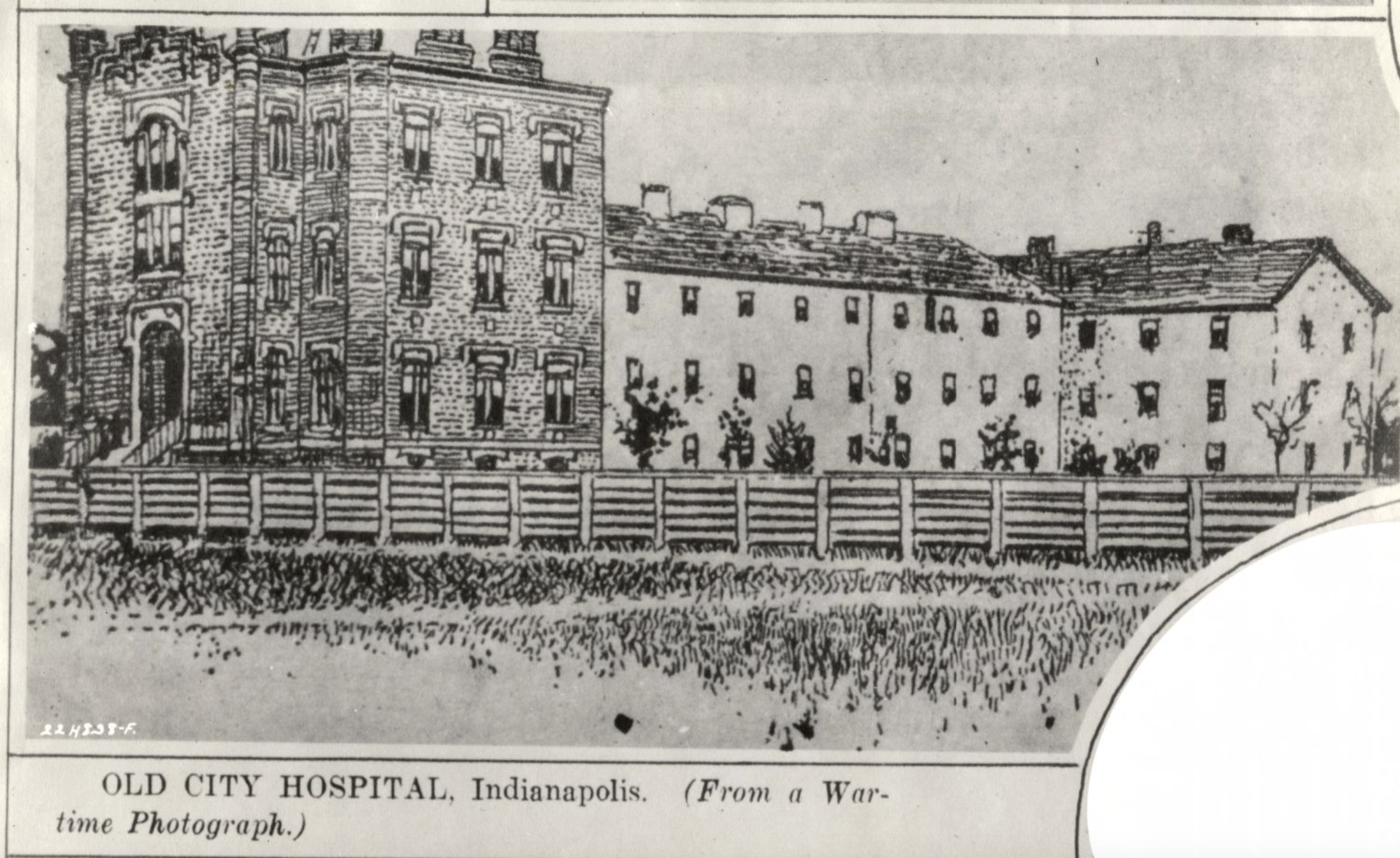
Indianapolis opened its first hospital during the . The Indianapolis City Hospital (later ) was used by the federal government to care for sick and wounded soldiers. After the war, the city assumed control of the facility and operated it as a charity hospital that provided care for the indigent. Like city hospitals elsewhere, the institution was constantly overcrowded and chronically underfunded.
The late 19th and early 20th centuries witnessed the expansion of City Hospital and the opening of a number of other hospitals to provide better care for those considered the worthy poor, as well as for paying patients. The Daughters of Charity of the St. Vincent de Paul Society established the St. Vincent Infirmary (later ) in 1881. In 1899 the German Protestant Deaconess Hospital and Home for the Aged (later known as the Indiana Christian Hospital and Clinic) opened. The Epworth League dedicated its 65-bed Methodist Episcopal Hospital (later ) in 1908. Although all these institutions initially accepted charity cases, the majority of the patients paid for care and consequently the care at these institutions was superior to City Hospital. These new hospitals and hospital additions employed the latest techniques in hospital architecture. Most were laid out in a pavilion style, which maximized ventilation, minimized the crowding of wards, and reduced the risk of infection. Pavilion hospitals usually were sprawling structures, one or two stories in height.
By the early 20th century, much of the stigma attached to hospitals had subsided. Hospitals began offering specialty services such as care for contagious patients, obstetrics-gynecology, ophthalmology, gastroenterology, neurology, and urology. Hospitals were also influenced by the tremendous growth of medical science (especially the development of the germ theory and bacteriology) and medical technology improvements in medical education, and the professionalization of nursing. For the first time, hospitals had the potential for providing better care than could be received at home. They also became an integral part of the medical education system and important facilities for training medical students and nurses, as well as major research centers.

As the demand for hospital services rapidly increased, Indianapolis hospitals could not keep pace with the need for bed space. In 1914 the Poor Sisters of St. Francis Seraph of Perpetual Adoration founded . This 75-bed charity hospital served the city’s rapidly expanding south side and eventually accepted mostly paying patients.
The 1910s and 1920s also witnessed the growth of a number of specialty hospitals funded through private philanthropy. The Robert Long Hospital opened in 1914 as a 138-bed hospital for the care of the rural poor. Although Long donated the original gift for the hospital, the institution relied on the state for operating support. Because of a generous gift from William H. Coleman and his wife, the William H. Coleman Hospital for Women opened in 1927 to provide obstetrical and gynecological services. Through contributions collected by the Riley Memorial Association, the opened in 1924. Long, Riley and Coleman were all used as teaching hospitals for the .
During this time, two hospitals served the needs of the mentally ill. The Indiana Hospital for the Insane (later ) opened in 1848 as a state-funded hospital. This hospital remained open continuously to the early 1990s. In 1992, after several scandals and patient deaths at the institution, the governor ordered the facility to close. In 1899 the city opened the Marion County Insane Asylum (known as Julietta) and operated it until 1938. , founded by Albert Sterne, operated in the city’s near east side from 1898 to 1957 as a private facility to care for nervous and mental disorders. The latter was the first institution in the state to employ insulin, Metrazol, and electric-shock therapy
Despite all the hospitals in the city, the Black population failed to receive proper health care, since Indianapolis City Hospital was the only institution until the 1940s which admitted them. Unable to gain admission to existing hospitals, African Americans established their own hospitals, including (1909), Charity Hospital (1911), Dr. Ward’s Sanatorium (late 1910s; later Dr. Batties’ Sanitorium), and Provident Hospital (1921). All these institutions were short-lived since they lacked money and proper facilities to practice modern medicine. In 1927 the Black physicians of Indianapolis approached the to study the state of Black health care in the city. The foundation’s report in 1930 concluded that Indianapolis City Hospital’s facilities were woefully inadequate to care for Black residents, and it urged that City Hospital construct a separate hospital for them.

The Great Depression had an adverse effect on the city’s hospitals, with resources strained to the limit as charity care increased dramatically. Some hospitals were unable to withstand economic hardships. In 1935, after a number of reorganizations, Protestant Deaconess closed its doors. Other hospitals began considering accepting hospitalization insurance, although the state and local medical associations initially opposed it. In 1944 Methodist Hospital became the first Indianapolis hospital to sign an agreement with the Blue Cross Hospital Service.
The world wars also had an effect on local hospitals, especially with staff shortages. After World War I, many individuals became aware of the need for a hospital to care for the veterans. donated land on the near northwest side of the city (on Cold Spring Road) for such a facility. Originally called the General Medical and Surgical Hospital, it opened in 1932 as a model veterans’ hospital. In 1952 a new veterans facility opened near the medical school complex. The Cold Spring facility was used briefly for the care of tuberculosis patients. By the 1990s, both facilities were used for veterans and, although federally funded, both were an integral part of the Indiana University Medical School complex.
The end of World War II marked the beginning of the baby boom, which resulted in a need for more bed space. Demand for hospital bed space also occurred because of the growth of hospital insurance and the advances made in surgery.
Concerned about the lack of hospital bed space, the urged the community to take action. In 1951 a group of local businessmen formed the Indianapolis Hospital Development Association and named Edward Gallahue as its president. This represented the first attempt to systematize hospital development within Indianapolis. After assessing the city’s hospital needs, the association undertook a $12 million campaign to add 825 hospital beds by 1975. To participate in the campaign, however, hospitals could not discriminate by race. Hospitals which had previously not admitted Black residents (e.g., Methodist, St. Francis, Norways) began admitting them. The 1963 explosion at the Coliseum also pointed to the need for additional hospital bed space within the city.

Out of this campaign, many local hospitals added bed space. Also, opened in 1956 as a 300-bed facility. The money for that hospital was raised exclusively through private donations from eastside residents. In 1952 the state opened the first psychopathic hospital, , and opened a new facility on the medical school campus in 1971. Also, in 1956 Dr Joseph E. Walther founded Winona Memorial Clinic (later ), a voluntary hospital funded totally through private donations. Winona specialized in medical and surgical cases. In 1964 construction was begun on a much larger facility (280 beds) just north of the clinic. Although the construction of Winona Hospital increased the bed space in Indianapolis, it was not part of the citywide fund-raising campaign for hospitals.
In the 1960s, with the enactment of Medicare (1965), the health care industry witnessed dramatic growth. The government paid for the medical care of the elderly, and physicians set fees arbitrarily. The result was increased hospital admissions, new clinics, and skyrocketing medical costs. Health insurance premiums rose dramatically.
To control costs, the federal government in 1983 set prices in advance based on the expense of medical procedures. To implement this, they established diagnosis related groups (DRGs). DRGs created problems for the hospital and for the physician. If a person took a longer period of time to recover from an illness, the hospital paid the difference. As a result, hospital admissions declined, and the city was left with excess bed space.

Thus, 1983 and 1984 were very lean years for local hospitals; many cut staff or downsized their operations. Other hospitals sought new markets, offering specialized medical care and wellness programs. Methodist, the largest hospital in Indiana, became known for its treatment of heart disease, cancer, and diabetes, its emergency medicine and trauma center, the Midwest Eye Institute, and organ transplantation. Indiana University Hospital and Medical Center specialized in cancer, cardiac, and neonatal care, treatment for hypertension, neurosurgery, and rheumatology. St. Vincent Hospital became recognized for its heart institute, family life center, vascular center, and the specialties of sports medicine, oncology-biotherapy, geriatrics, and occupational health. Community Hospital’s specialties included neurology, cardiovascular programs, and oncology. Wishard Hospital’s burn and trauma units were among the best in the nation. The Winona Memorial Hospital had the , adult, child, and adolescent psychiatric services, and a diabetic unit.
The 1970s and 1980s also saw the development of a number of specialty hospitals including Westview (opened in 1975, now closed) for osteopathic medicine, New Hope of Indiana (a treatment facility for mentally and physically handicapped children that opened in 1978), Humana Women’s Hospital (the first for-profit hospital, which opened in 1983, now the Women’s Hospital-Indianapolis), Lifelines Hospital (opened in 1987 as a pediatric rehabilitation hospital), Fairbanks Hospital for the treatment of alcoholism, and Charter Hospital (a private hospital specializing in mental health and substance abuse treatment). The major hospitals like St. Vincent and Community opened “branch” hospitals in high-growth areas of the city and surrounding counties. They also opened community health centers and began utilizing outpatient departments to make their health care services more accessible.
*Note: This entry is from the original print edition of the Encyclopedia of Indianapolis (1994). We are currently seeking an individual with knowledge of this topic to update this entry.
Help improve this entry
Contribute information, offer corrections, suggest images.
You can also recommend new entries related to this topic.